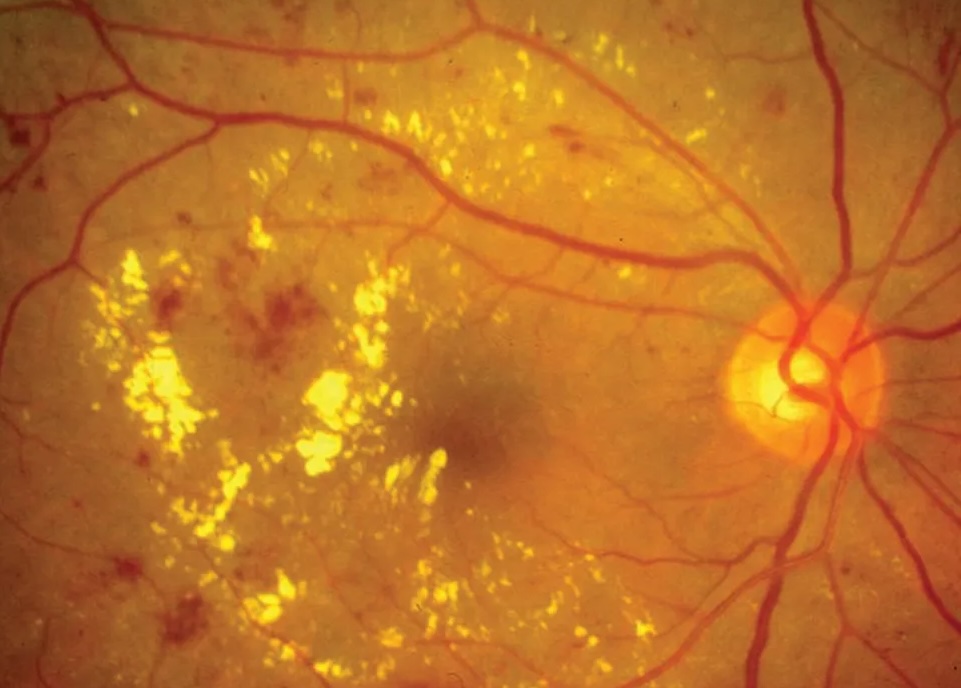
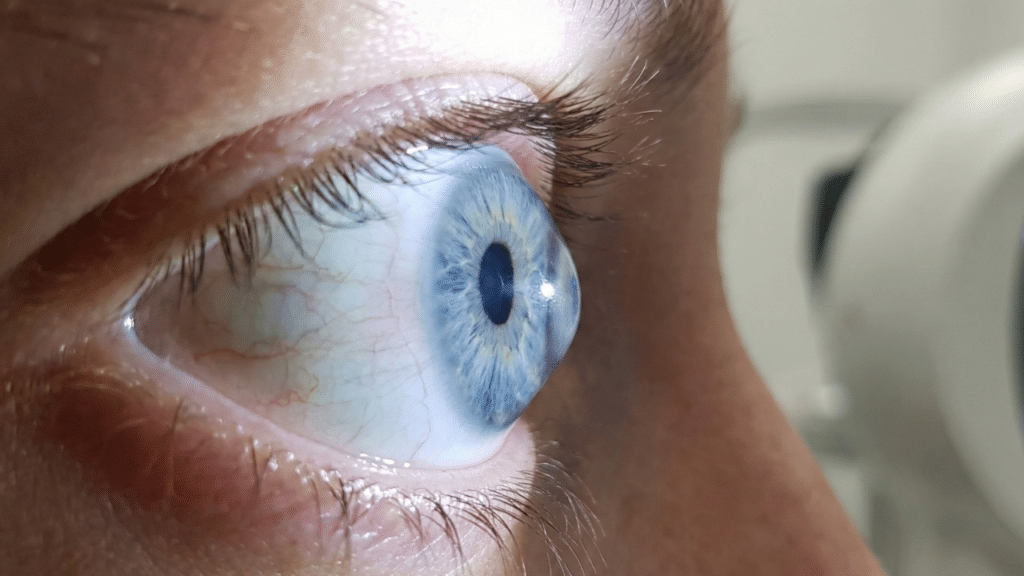
Biological Mechanisms of Vision Loss
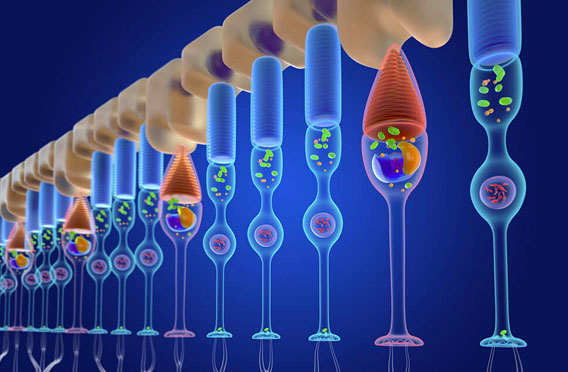
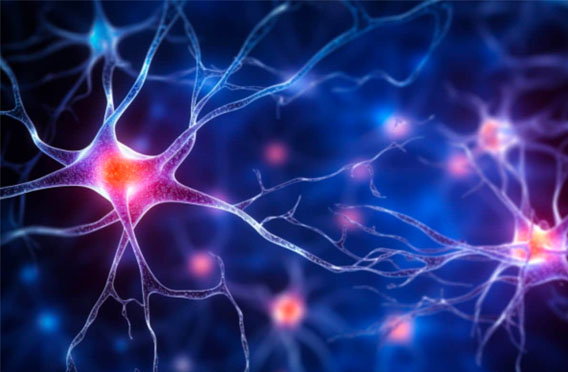
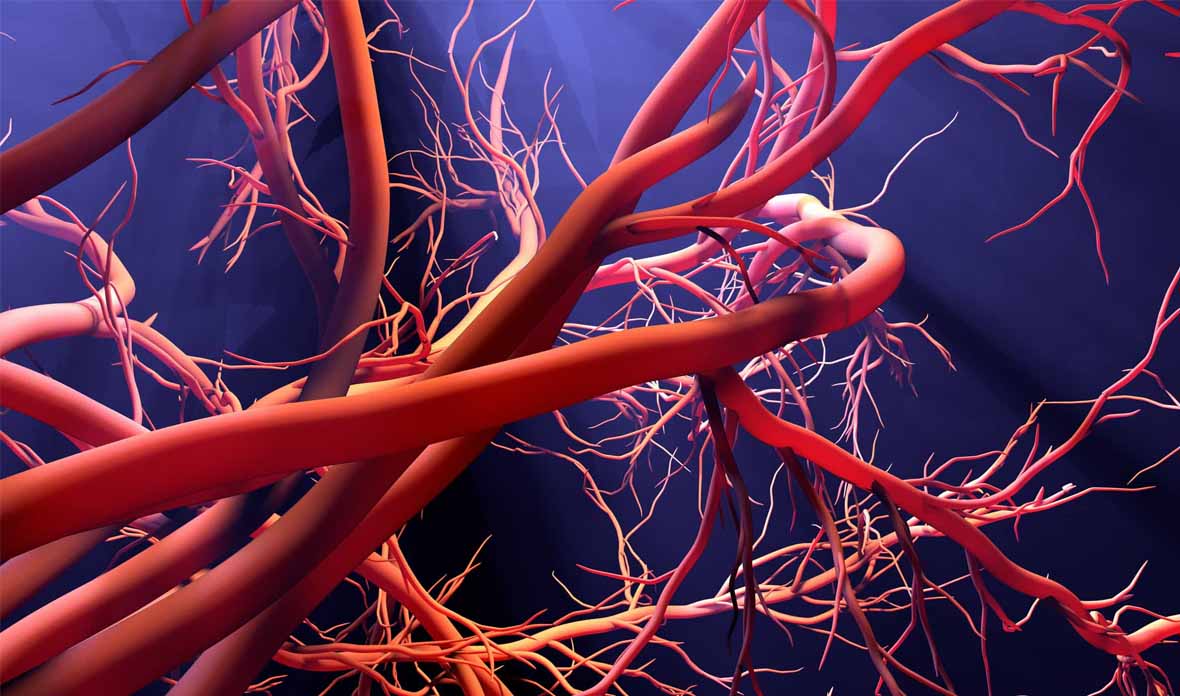
Vision loss results from interconnected biological disruptions affecting the retina and optic nerve. Reduced blood flow, impaired neurotrophic support, chronic inflammation, oxidative stress, and abnormal cellular signaling weaken neuronal survival and repair.