Beyond Cross-Linking: A New Way of Thinking About Keratoconus
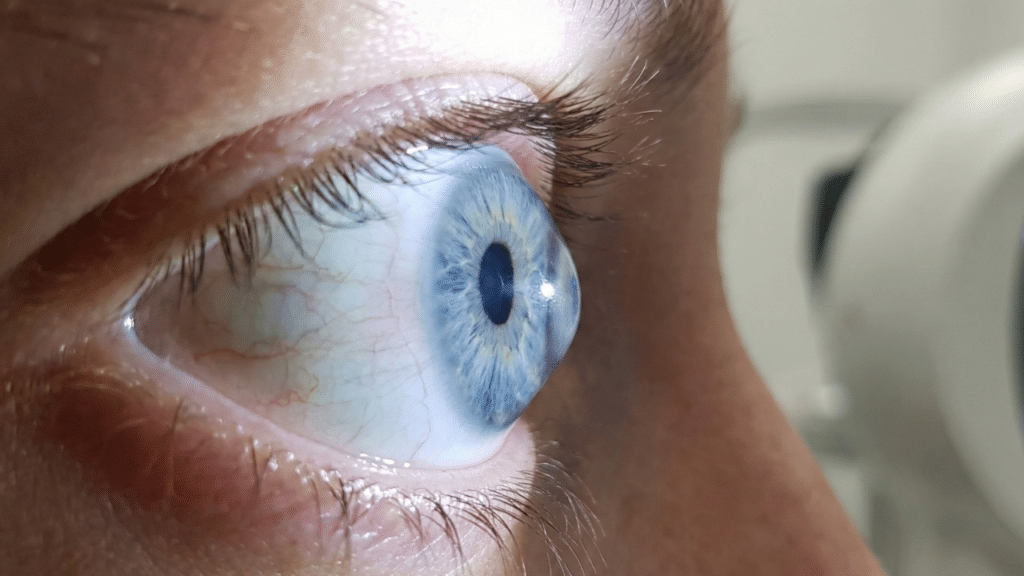
For years, people diagnosed with keratoconus were told the same thing: their corneas were structurally weak. The progressive eye disease, which causes the cornea to thin and bulge outward, was treated as amechanical problem, managed with rigid contact lenses, surgical implants, or a procedure called corneal cross-linking that stiffens corneal tissue. But scientists are now rethinking that explanation.
A growing body of research suggests keratoconus may not be simply a structural defect at all. Instead, many researchers now believe iti s driven by chronic inflammation and immune system activity inside the eye,even though the disease shows few outward signs of Inflammation.
That shift in understanding could explain why some patients continue to lose vision despite receiving standard treatments and why new approaches are beginning to focus on inflammation rather than shape alone.
The Inflammation YouCan’t See
Keratoconus does not usually cause redness, swelling, or pain. That’s one reason it was long considered non-inflammatory. But modern laboratory techniques tell a different story.
Studies examining tear fluid and corneal tissue in keratoconus patients consistently find elevated levels of inflammatory molecules, known as cytokines. These include interleukin-6, tumor necrosis factor-alpha, and otherimmune signals commonly associated with tissue Damage.
Researchers have also found that higher levels of these inflammatory markers often correlate with more severe disease. In other words, while the eye may look calm on the surface, immune activity beneath it appears to be quietly weakening corneal tissue over time.
How InflammationWeakens the Eye
The cornea maintains its strength through a precisely organized collagen framework. Chronic inflammation disrupts this framework by activating enzymes that break down collagen faster then the eye can repair it.
Mechanical stress, such as frequent eye rubbing, often associated with allergies or dry eye, can intensify the inflammatory response.Each episode of rubbing triggers additional cytokine release, creating a feedback loop that accelerates corneal thinning and distortion. Over months or years, this process leads to the cone-shaped bulging that defines keratoconus.
Oxidative Stress andCell Damage
Inflammation is only part of the story. Researchers have also identified oxidative stress, a form of cellular damage caused by unstable oxygen molecules, as a major contributor to Keratoconus.
In healthy eyes, antioxidants neutralize these molecules.In keratoconus patients, antioxidant defenses appear impaired, allowing damage to accumulate. This environment can trigger ferroptosis, a recently recognized form of cell death that destroys corneal cells essential for maintaining tissue strength. Together, inflammation and oxidative stress create conditions in which the cornea steadily loses its ability to maintain its shape.
Why Some TreatmentsDon’t Stop Progression
Corneal collagen cross-linking remains one of the mostwidely used treatments for keratoconus. By stiffening collagen fibers, it can slow disease progression for many patients.
But long-term studies show that as many as one in five patients continues to worsen even after cross-linking. Researchers increasingly believe persistent inflammation may explain why. While cross linking addresses the cornea’s mechanical weakness, it does not directly target the immune and biochemical processes that continue to degrade tissue. But there are some types of treatment of keratoconus in Ayurveda that help in slowing down the progression or at least limit the progression.
A New Focus onRegulating Inflammation
As understanding of keratoconus evolves, some clinics and researchers are exploring treatments designed to regulate ocular inflammation and cytokine activity, rather than focusing solely on reshaping or stiffeningthe cornea.One such approach is Corneal Cytokine Regulation (CCR), a treatment model offered by Netra Eye Institute, a specialty holistic eye center that emphasizes non-surgical management of complex eye diseases.
According to the clinic, CCR is designed to address the biological processes increasingly linked to keratoconus progression, specifically chronic inflammation, oxidative stress, impaired ocular blood flow, and inflammatory cell signaling. The approach integrates therapies aimedat calming immune activity, supporting antioxidant defenses, and improving the eye’s metabolic environment.
Unlike conventional treatments that focus primarily on corneal structure, CCR at Netra Eye Institute targets cytokine imbalance, which many researchers now view as a central driver of corneal degeneration in Keratoconus.
What This Means forPatients
For patients, the growing recognition of keratoconus asan inflammatory disease may expand treatment options, especially for those who continue to progress despite standard care or who are seeking non-surgical alternatives.
Experts caution that inflammation-focused therapies are still part of an evolving field, and continued research will be essential. But the shift itself is significant.
As scientists continue to unravel the immune, oxidative, and vascular factors involved, the hope is that treating keratoconus at its root, not just managing its physical consequences, will lead to better long-term vision outcomes for millions worldwide.
Frequently AskedQuestions
What is the newest approach to treating keratoconus?
New research views keratoconus as an inflammatory condition, not just a structural problem. holistic keratoconus treatment focuses onreducing inflammation, oxidative stress, and immune imbalance rather than only reshaping or stiffening the cornea, offering a more root-cause–based approach.
Can inflammation really cause keratoconus to worsen?
Yes. Studies show elevated inflammatory cytokines in keratoconus patients, even without visible redness. Chronic inflammation weakens corneal collagen over time, accelerating thinning and bulging. This explains why some patients continue progressing despite standard mechanical treatments like cross-linking.
Why doesn’t corneal cross-linking always stop keratoconus progression?
Cross-linking strengthens corneal fibers but does not address ongoing inflammation or oxidative stress. If immune activity continues,corneal tissue can still degrade. This is why some patients explore holistic keratoconus treatment options that aim to regulate biological and inflammatory processes.
Is there a role for Ayurveda or acupuncture in keratoconus care?
Some patients explore complementary approaches such as treatment of keratoconus in Ayurveda and acupuncture for keratoconus treatment aspart of a holistic care plan. These systems aim to support inflammation balance, circulation, and overall eye health, alongside conventional monitoring.
Who may benefit from inflammation-focused keratoconus treatments?
Patients with progressive keratoconus, ongoing eye rubbing, allergies, or worsening vision despite standard care may benefit most.Holistic keratoconus treatment approaches are often considered by those seeking non-surgical options or additional support beyond contact lenses or cross-linking.